***********************
If You Are Having Suicidal Thoughts Read This First
***********************
This episode recounts my experiences of the NHS when I sought help because I was contemplating suicide. The NHS response recounted here is based on their clinical assessment that whilst genuinely feeling like I wanted to take my own life, they felt I was not at immediate risk of doing so. Their subsequent response after their initial assessment has been painfully slow and it looks like I won’t get the help they think I need for 7 months. However had I been a high risk, their initial triage response would have been completely different and steps would have been taken immediately to help me.
So if you are having suicidal thoughts and think the NHS will respond to you like they have done for me and that contacting them might not seem worth it then still go and let professionals identify how much of a risk you are. You are probably not in the right frame of mind to make that decision – I know I wasn’t. And even though I am still searching for ways to heal the suffering I’ve been through, going to my doctor and asking for help, as difficult as it was for me, has been the start of my turnaround – even if I am just taking those first stumbling steps.
I don’t know you, you don’t know me, but if you’re here reading this then we probably share similar pain and I deeply care about that. I understand how it feels, I felt the same way and despite my deep seated fears and reservations, I found that asking for help, even though not necessarily receiving it, has been a lifesaver. This blog is about reaching out to myself, but it is also about reaching out to you.
Don’t be surprised if you see this message at the end of this post – it’s that important!
Podcast Summary
In this episode I share what has happened since I went to my GP and asked for help because I wanted to take my own life.
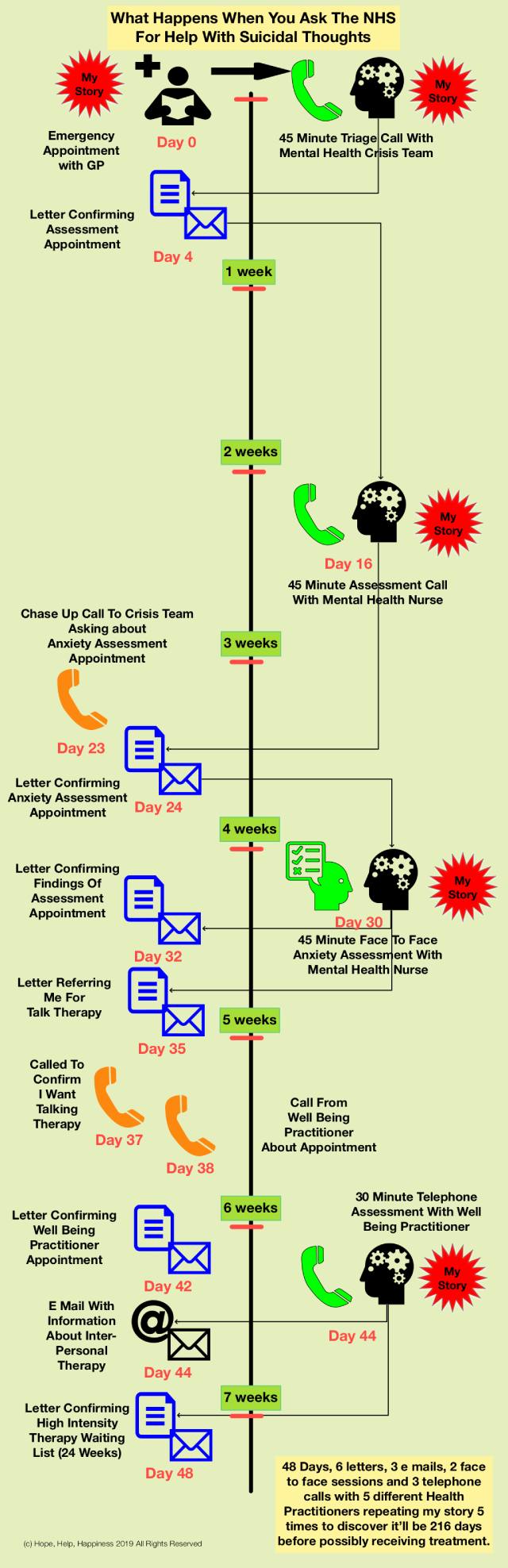
It has taken 48 days, 6 letters, 3 emails, 2 face to face sessions and 3 telephone consultations with 5 different health professionals (two lasting 45 minutes and one of 30 minutes) to discover it will be at least 216 days (31 weeks or 7 months) from asking for help to possibly getting to the top of a waiting list for treatment.
I have repeated my story of suffering 5 times to 5 different people and still after 7 weeks, I am no further forward.
Podcast Transcription (Edited)
Welcome to this episode of the Hope, Help, Happiness podcast where I am recording my journey through dealing with the problems initially of feeling suicidal and the desire to take my own life through to hopefully some form of future happiness.
Now I wanted to use this episode to give a record of the journey I’ve taken so far in going to the National Health Service through my GP and asking for help. It’s been an interesting journey going through the process of especially in asking for help, which in itself was a huge step for me because of challenges I’ve had in the past.
There’s been a lot of activity but very little progress. And I think what has come to light from the experience for me is that I really can’t rely on the health service to support me in my journey to recovery. And let me explain why.
The problems I’ve been having as part of my whole life experience, result from having a tendency to be more melancholic. And that means I have a generally pessimistic view on life. Coupled with the problems I now realise have been caused by low self-esteem, I have been more prone to bouts of depression.
Coupled with all the life experiences I’ve had has meant I’ve been somewhat down over the last couple of years. There’ve been some significant challenges in my life I’ve struggled to deal with and they’ve had a negative impact on my mental, emotional, and I suppose my physical health. To the point, certainly over the last year, I’ve been feeling my life wasn’t worth living, that I couldn’t move forward and that it was a real struggle.
Over the last year, I’ve seriously contemplated taking my life to the point where I came very close to doing so. But I realised it was a difficult thing for me to do. I wasn’t brave enough to pull the trigger, metaphorically speaking. And so I tried again and tried again to manage my mental and emotional state.
Then in the run up to my birthday, I found myself getting more and more despondent to the point where I was at the point where I could see no way out.
I’m just explaining this again to you because I want you to get a sense of the emotional distress I found myself in at the point of me going to my doctor and asking for help. It was a huge step for me and I’ll talk about that later on in a future episode.
I asked for help because of the realisation I didn’t have the courage to go through with it, but also because of the genuine love and affection I received from a couple of people who unwittingly don’t realise just how much they have contributed to probably saving my life.
I am about to explain my experiences. Here’s an infographic I put together to illustrate my experiences and to give a sense of the timeline associated with them.
I realised I needed to do something that morning so I contacted my doctor’s surgery. Let’s call that day Zero for the purposes of my timeline. First of all I had to ring up my surgery and say I needed a emergency appointment. They asked why and I felt embarrassed to explain it was because I’d had thoughts of suicide.
They rang me back within 30 minutes to say, yes, come on in. I think the appointment was about an hour after they called. They encouraged me to make my way to the surgery before the appointment. So I went to the doctors and sat in their waiting room. I had to wait for about 25-35 minutes or so before the doctor saw me.
She asked what the problem was and I basically blurted out how I was feeling. It was an emotional situation. She was very compassionate and listened. As a result of our conversation, she contacted the Mental Health Crisis Team and ask if they could speak with me then.
If I take myself outside of those circumstances for a minute, I realise now that the doctor’s role there is to see whether I presented a risk in actually doing some harm to myself or even other people. And so her job is to triage that risk and see whether there’s anything to worry about.
Clearly she thought there was, because she referred me to the crisis team.
She had to ring them so whilst she did I had to sit in the waiting room for some time. Eventually she came back and said she’d managed to get a telephone appointment with the team, but I still had to wait something like an hour. So I sat in the waiting room which was an interesting experience watching people of all ages come and go.
I haven’t been to the doctors for a very long time. Well the last I went to the doctors was five years before to register with this practice when I moved to the area. I pride myself in looking after my physical health and, and am generally in good shape so I don’t need to go to see the doctor.
Eventually I was given a private space where I had a 45 minute call with a lady from the mental health crisis team. Now I think she was a nurse and she explained her role was to assess whether I was a risk to myself or to others and basically asked me what the situation was.
I then spent 45 minutes repeating much of what I’d already told the doctor but in a little bit more detail. The conversation was a useful outlet for me. It allowed me to burst the bubble that had been building up inside of me over the previous weeks and months. I’d Isolated myself and allowed negative thoughts to swirl around in my mind unchecked, getting bigger and bigger and bigger and bigger.
And so actually talking through the problems, expressing them was a release, almost a form of therapy in its own right.
We had a conversation and she showed a lot of empathy and a lot of compassion which really did help. We basically talked about what I needed to do move forward. She recommended that I take antidepressants. I said I didn’t want to. I think I’ve explained my reasons for that, but I might explore that further in another episode.
At the end of the call she said she’d set up a proper assessment appointment. So I suspect that at that point she realised I wasn’t a threat to myself or anyone else. And so she basically put me into the system.
Straight after that, after being in the system for just a day, a letter is written telling me about an assessment appointment – a screening meeting I suppose to basically identify what help I needed now. I received the letter probably two or three days later.
And so the way I felt at that moment, was that things might be okay – some sort of progress was being made. But I was still in a sort of limbo state because I didn’t know what was going to happen. But I knew something was happening. So I felt somewhat reassured but didn’t know exactly what the appointment, scheduled for two weeks later, was about.
One thing that did concern me was the length of time between asking for help and the first step on a potential journey to recovery.
On day 16 after my first contact with the health service, I had a 45 minute telephone call with someone new, a different mental health nurse to the one I’d previously spoken to. Beforehand I’d written down all the issues and the concerns and the challenges I was facing together with some of the background on a piece of paper. So I was prepared to be able to explain what was going on, but essentially it turned out to be a repeat of the two conversations I’d already had before.
So we had this 45 minute conversation and again, it was productive. It was compassionate, it was positive, and there seemed to be some form of progress being made. The recommendation I was given was that she felt I’d benefit from antidepressants. I flatly refused and explained why.
Based on the conversation she didn’t feel CBT (Cognitive Based Therapy) was the right thing for me and felt that counselling was the best way forward for me. Unfortunately, counselling is not available on the NHS, so I’d have to fund that privately. She recommended a local counselling service and suggested I contact them. I did and I’ll share more about that later on.
One of the things she also said, based on the questionnaires I had to fill out before the call and from some of the things I’d said, was there might be issues of anxiety. So she recommended I have an appointment with one of her colleagues who would do an anxiety assessment. She promised to set that up.
All this happened on day 16 after my first contact with the health service. I still hadn’t heard anything about the next appointment nearly a week later, so I contacted them and to my surprise I managed to speak to the same nurse again. I told her I’d not heard anything but she promised her colleague would get in touch with me soon.
The following day I received a letter which had been dated three or four days beforehand but just probably hadn’t been posted. So the letter was the schedule for an appointment the following week.
That meant another wait. On day 30, this is two weeks after I’d had the assessment interview, I then had a face to face with another mental health nurse. We had a 45 minute conversation. What was interesting was I’d assumed my anxiety levels will be tested because that’s what I was told. But I just had another 45 minute conversation with someone new, where I pretty much had to repeat what I’d already told the three previous people I’d spoken to.
I didn’t seem to be making much progress. I just seemed to be getting better at telling my story.
One or two interesting things came out. She started looking into why I might be suffering with the challenges I am having and recommended I look up attachment theory. She did say she wasn’t a therapist but offered me that advice anyway.
She ended the conversation at the allotted time and promised she’d take what she could from the meeting and was going to talk to her supervisor to explore a way forward. That day she wrote a letter to me and recommended that I have an assessment for interpersonal therapy.
So that’s day 30 and still, I haven’t got any guidance or any support on dealing with the challenges I’m facing.
On day 35, I received a letter saying I’ve been referred to a talking therapy service. This letter basically said there’s an assessment on offer after which they’ll follow and provide a treatment plan, and I needed to get back to them to set it up if I still wanted the support.
I rang them back and was told that a wellbeing practitioner would call me. So now this isn’t a nurse dealing with my issues anymore. I don’t know what a wellbeing practitioner is, but they would ring me.
I did get a call from them on day 38 saying they were going to set up an appointment and then on day 42 I received the letter that set up the appointment. And then on day 44, I finally had a telephone conversation with the psychological wellbeing practitioner. It was a 30 minute call. Again, I had to go through the same explanation of what my challenges were. First he went through a mandatory risk assessment, asked about my history and more general questions about my health. And then went into looking at the challenges I faced.
He fed back that I needed to be more compassionate with myself and that I probably needed a structure in which to move forward. He ended the call after 30 minutes and said he would need to talk to a supervisor.
Later that day, he called me back and said that he was recommended me for interpersonal therapy and promised to send over an email with some explanatory information.
…But it wouldn’t be available for 15 to 20 weeks!
So six weeks after my first interaction with the health service, I’m told that I’m not going to get any help for another 15 to 20 weeks.
I received a follow up letter which arrived on day 48. It summarised the scores from the questionnaires I had filled in prior to the appointment, confirmed they didn’t identify me as a risk and outlined the way forward.
The statement that I was most interested in said this:
“We agreed that you would like to have face to face high intensity psychological therapy with a high intensity therapist.
Now this is a new term for me because he talked about interpersonal therapy and he’d sent me an email with information about interpersonal therapy. So all of a sudden now I’m being recommended for high intensity psychological therapy.
Because the words are different I’m assuming they are different things. But it’s not clear what that is. And I don’t remember agreeing to that because it’s the first time I’d seen that term.
That aside, here’s the kicker.
I have to go on a waiting list and I understand that because the world doesn’t revolve around me. But the anticipated start of my treatment is approximately 24 weeks away (not the 15-20 weeks he promised on the telephone) .
So 216 days after me wandering into the GP’s surgery in an emotional distressed state, wanting to take my own life, I won’t be receiving any treatment for 216 days.
That’s 31 weeks!
That’s seven months!
I am struggling to cope with day to day life – day to day activities. I know I have learned helplessness. I know got all these issues. I’m really struggling to make any progress. The people close to me can’t see that because I mask it because I don’t want to reveal the challenges I’m facing.
No one can really help me. I’ve got to deal with it myself. I realise that, but I do need help to be pushed along. That’s why I approached the health service. I’ve been paying my taxes, my national insurance into the health service all these years. And now when I want something from it, I’m going to have to wait 216 days from needing it.
I must stress, the people who I’ve had contact with have been very professional, very well meaning and on the whole came across as very supportive. But from this response, it appears the system isn’t going to or can’t help me handle the challenges I face, when I need to face them.
And so I’ve got to do something about that and I am going to do something about that.
But I think it’s just really interesting that there maybe people out there who may not be quite so proactive as I am going to have to be, who may also be faced with this delay. How might they handle it. It worries me.
So it’s taken seven weeks to get some sort of progress and even then I still face a significant delay. If I had the money, of course I could just go and pay for this. I don’t want to knock the health system because it is under enough strain as it is. What this is for me, what I’ll take from this is I can’t rely on anyone else to fix me.
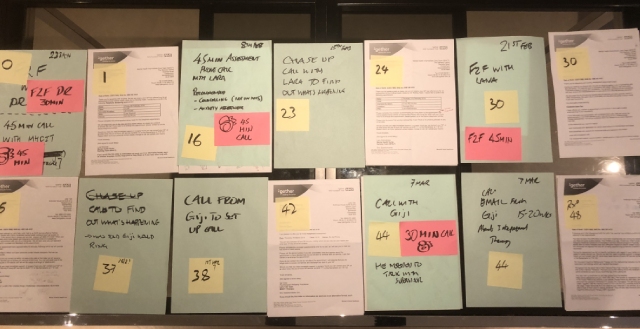
Here’s a photograph of all the NHS administration involved in dealing with me in the last 7 weeks.
I have to take responsibility for my own mental health and the healing process I’ll need to go through. I was hoping I’d get a little bit of support and the health service can give me something but not for another seven months after I really need it. By then I may not even need it… or it might be too late!
But I don’t know. I’m still going to go forward with this to see where it takes me.
An Alternative Journey – Counselling
Let’s go back for a moment to day 16 when I was recommended counselling, a treatment that’s not available on the NHS. I did contact the local counselling service and they recommended I go to their website to fill out a form to explain what was going on. I did and paid £50 for an assessment appointment. They confirmed my interest in their services with an automated e mail and promised they’d contact me soon with an appointment.
Five days later I get an email saying I have an appointment four weeks away. And again, I had the same feelings as I had with the slow time response from the NHS. I need support and I really need it now. Just to contact them I’ve broken through my own massive inner resistance to asking for help.
And then having trusted and broken through that resistance, I’m disappointed I can’t receive it support when I really need it.
So I rang them up, explained my predicament and asked if there was any possibility they could bring that forward? And they said yes. They brought it forward a week. The administrator I spoke to was very helpful and I was very grateful for them doing that.
Last week I had the assessment interview where once again I had to explain what I was going through to a trained counsellor. This is the 6th time I have shared my story in the last 6 weeks. She promised to take my case to their weekly planning meeting and hopefully I’d be allocated a therapist soon.
They called me a couple of days ago to tell me I’d been allocated a therapist. In fact, it was the therapist who did the assessment and at time of writing this, I’ve got an appointment with them in about an hour and a half’s time. I’m delighted it’s going to be the same person I’ve already spoken to. At last some consistency (this will be the 6th person, other than administrators and reception staff, I’ve dealt with in the last 7 weeks)
I’m going to go through with the therapy. Not quite sure how I’m going to pay for that at the moment because of the way I’m struggling to generate income under of all the challenges I’m facing. But that’s a problem I’m going to have to face up to it.
This post has been about sharing the difficulties I have had in getting help from the NHS. I’ve had similar problems before and wanted to share them here. I am struggling with the challenges I face at the moment so whilst these delays are typical, they are not helpful.
If I take the positive view of this, at least it is going to give me a kick up the backside and make me seek my own solutions.
Now I’m off to my first counselling session and I’ll probably tell you about that tomorrow.
So until tomorrow.
***********************
If You Are Having Suicidal Thoughts Read This First
***********************
This episode recounts my experiences of the NHS when I sought help because I was contemplating suicide. The NHS response recounted here is based on their clinical assessment that whilst genuinely feeling like I wanted to take my own life, they felt I was not at immediate risk of doing so. Their subsequent response after their initial assessment has been painfully slow and it looks like I won’t get the help they think I need for 7 months. However had I been a high risk, their initial triage response would have been completely different and steps would have been taken immediately to help me.
So if you are having suicidal thoughts and think the NHS will respond to you like they have done for me and that contacting them might not seem worth it then still go and let professionals identify how much of a risk you are. You are probably not in the right frame of mind to make that decision – I know I wasn’t. And even though I am still searching for ways to heal the suffering I’ve been through, going to my doctor and asking for help, as difficult as it was for me, has been the start of my turnaround – even if I am just taking those first stumbling steps.
I don’t know you, you don’t know me, but if you’re here reading this then we probably share similar pain and I deeply care about that. I understand how it feels, I felt the same way and despite my deep seated fears and reservations, I found that asking for help, even though not necessarily receiving it, has been a lifesaver. This blog is about reaching out to myself, but it is also about reaching out to you.
See I told you you’d see this message at the end of this post – it is that important!